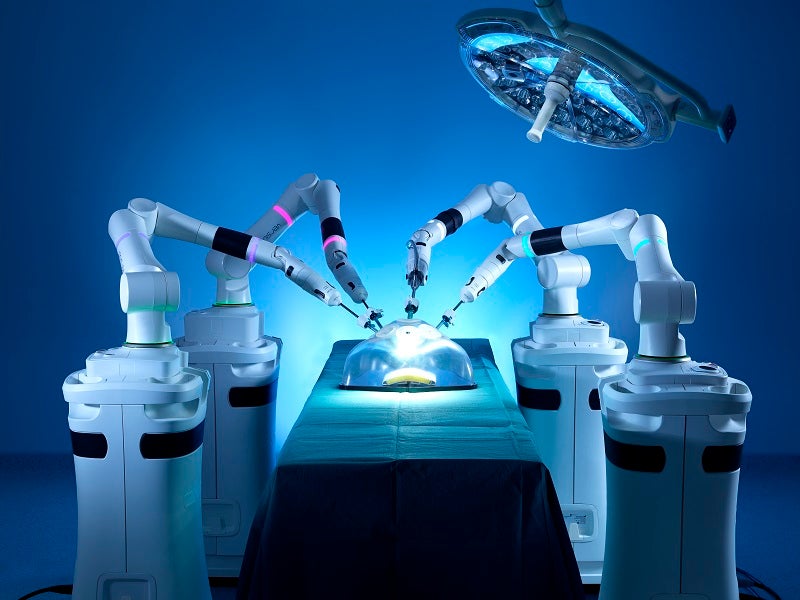
Emerging technology Robotic Bariatric Surgery
The robotic platform has now proven to be as safe and effective as the traditional laparoscopic procedure, which has propelled the practice and safety of bariatric surgery.
February 3, 2022
Written by: Dr. Samir Patel
The prevalence of morbid obesity continues to increase in the United States and throughout the world. In the US, 65% of the adults are classified as either overweight (body mass index (BMI) >25) or obese (BMI>30). Most of that increase is in the obese population, with more than 6% of those being morbidly obese (a BMI>40). Advances in surgical technology have allowed surgeries to be performed safely with minimally invasive techniques. They have improved the outcomes of bariatric surgery to such an extent that bariatric surgery has now proven to be superior to intensive medical management in both weight loss and overall long-term mortality; even when factoring perioperative morbidity and mortality.
More than 200,000 surgical weight loss procedures are performed annually. The majority of these being the sleeve gastrectomy (58.1%), followed by the Roux-en-Y gastric bypass (18.7%), and a fast-rising rate of bariatric revisional surgery (13.9%). The National Institutes of Health (NIH) consensus statement of 1991 states that a patient is a candidate for surgery if they have a BMI>35 with an obesity-related co-morbidity (i.e.- hypertension, diabetes mellitus, sleep apnea, coronary heart disease, gastroesophageal reflux disease) or a BMI>40 with no added co-morbidities. (1)
Both the sleeve gastrectomy and the Roux-en-Y gastric bypass are performed laparoscopically, and more recently robotically. Studies comparing both laparoscopic and robotic surgeries have now shown equivalent morbidity and mortality, with similar weight loss results. However, technical issues can arise when operating on patients with a BMI>50 and beyond. These patients have anatomical challenges —such as thick abdominal walls (particularly female patients) which may require excessive torque to the laparoscopic trocars and instruments resulting in potential tissue trauma, less precise movements, and surgeon fatigue. There is also added difficulty in gaining pneumoperitoneum in the superobese patients thus requiring higher insufflation pressures and a smaller intra-abdominal working space which makes fine dissection difficult. The wristed, 3-dimensional movements and high-definition magnified view, achieved by the daVinci robotic instruments and cameras allows surgeon using this platform to overcome these technical challenges. Furthermore, the robotic arms have precise movements with enough mechanical power to minimize the torque required to maneuver surgical instruments and minimize the risk of trauma to the abdominal wall, resulting in less postoperative pain and a faster recovery. (2)
In my experience using both the laparoscopic and robotic platforms, I have found the stapler platform developed in robotics to be more “intelligent”. The built-in software affords the surgeon more information about the patient’s tissue leading to better staple size choice, resulting in a better-formed staple line with less intraoperative and postoperative bleeding. Having the advantage of 3D visualization of the anatomy during surgery allows me to manipulate the wristed instruments with finesse to perform a safer surgical procedure.
In conclusion, the robotic platform has now proven to be as safe and effective as the traditional laparoscopic procedure, which has propelled the practice and safety of bariatric surgery. I believe in its potential to improve postoperative outcomes as well as hasten patient recovery. I am excited to be a part of the growing number of bariatric programs around the country offering this cutting-edge new technology to our patients.
-
Rogers. A. and Lidor, A. “Management of morbid obesity”. Current Surgical therapy, pg 117.
-
Itum, D and Kukreja, S. “Robotic Sleeve Gastrectomy”. The SAGES Manual of Robotic Surgery, pgs. 115-116


